Oral Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2016
The 5:2 STOP Study: A pilot study to compare the metabolic effects and safety of weight loss via intermittent fasting versus standard continuous energy restriction in patients with Type 1 diabetes and overweight or obesity (#179)
Over 50% of our Type 1 diabetic population are classified as overweight or obese. The consequences of this excess body weight are well recognised. There is little data to support a particular dietary approach to weight loss in this high risk cohort. We therefore conducted a pilot study to compare the metabolic effects and safety of weight loss via intermittent fasting (IF) versus continuous energy restriction (CER).
Eight overweight or obese Type 1 patients were randomised to follow IF or CER for 12 weeks. IF participants consumed three VLED shakes (~2600 Kj/day), commencing at the evening meal for two 24-hour periods/week. CR participants were given individualised 2100 kj deficit/day diet plans. Basal insulin doses were initially reduced by 50% for IF days or 10% for CER. Weekly contact was maintained for insulin adjustment, and monitoring of ketones and glucose. Resting Energy Expenditure (REE), body composition (DEXA), continuous blood glucose monitoring (CGM) and pathology were performed at baseline and 13 weeks.
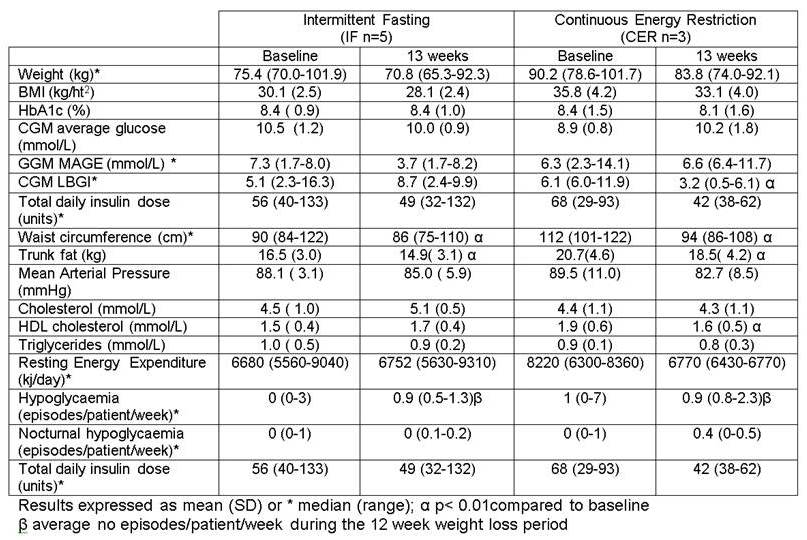
Relative to baseline significant weight loss was seen in both groups at week 13 (6.2% versus 6.7%) with no change in HbA1c (Table 1). There was a significant reduction in waist circumference and DEXA trunk fat in both groups. There was no change in mean arterial pressure, total cholesterol or triglycerides, although HDL cholesterol dropped in the CER group. REE remained unchanged. Hypoglycaemia was also unchanged however participants’ total daily insulin needed to be reduced by 16.4% and 33.3% respectively. Blood ketone levels reached 1.6 mmol/L in one IF participant, a level seen in some individuals without diabetes during ketogenic diets, but their blood ketone level fell below 0.4 mmol/L following the next meal.
CER and IF appear to be effective weight loss strategies for Type 1 diabetes, but close monitoring of insulin requirements and ketosis is required.