Poster Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2016
Patient and Healthcare Provider Attitudes Towards Insulin Therapy in a Tertiary Referral Hospital in South West Sydney (#347)
Background:
Delayed introduction of insulin therapy in people with type 2 diabetes mellitus (T2D) often prolongs duration of suboptimal glycaemic control, which in turn increases rates of complications. A leading perceived issue about insulin use, in both patients (Pts) and their health care providers (HCP), is the need to administer via subcutaneous injection. In this study we examined and compared attitudes towards insulin in both Pts and HCPs admitted / working in a large tertiary referral hospital.
Methods:
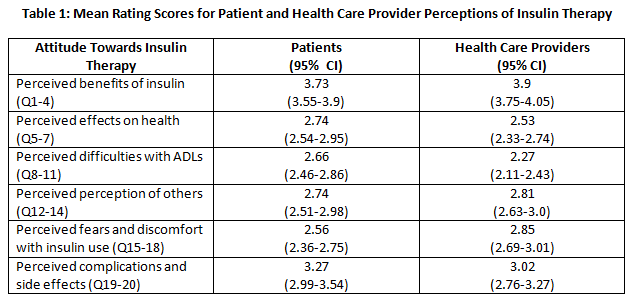
Thirty admitted Pts with T2D and 30 HCPs (14 junior medical officers and 16 registered nurses) completed a self-administered questionnaire: the “Insulin Perception Questionnaire”, which was adapted from the DAWN (Diabetes Attitudes Wishes and Needs) study. Both HCPs and Pts were randomly recruited (only Pts with T2D were enrolled) with all aged over 18 years and English language literate. Participants rated their disagreement or agreement (on a scale of one to five) to statements exploring their attitudes regarding the benefits of insulin, impact on their health, interruption of insulin therapy on daily living, perception by others, fears associated with insulin and perceived complications from insulin. Pts rated their own attitudes while HCPs rated their perception of attitudes of people with T2D under their care.
Results:
Pts non-significantly did not perceive the benefits of insulin as highly as HCPs (mean±SD: 3.73± 0.95 v 3.9 ±0.83, p=0.1313) but significantly their fear and discomfort from injections was lower than that perceived by HCPs (2.56±1.09 v 2.85±0.89, p=0.03).
Conclusion:
These results suggest that while patients may not understand the benefits of insulin therapy, they are actually more receptive to initiation than what is perceived by their HCPs. Hospitalisation may be an opportunity to review and individualise DM treatments, especially in regards to the timely commencement of insulin therapy.