Poster Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2016
Preventing Diabetes in people with Depression in primary health care (PDD trial): a pilot study (#305)
Background: Type 2 diabetes (T2D) is an increasing health and economic burden in Australia. We investigated the feasibility of conducting a full-scale study on the effectiveness of a multidisciplinary team-based model of care (‘Collaborative Care’) for preventing T2D in people with pre-diabetes and comorbid depression in primary health care.
Methods: We examined the feasibility of recruitment, participant retention, assessment procedures, and intervention fidelity in one GP practice located in South Western Sydney using a 12-week pre-test/post-test design. Post-test semi-structured interviews were used to explore views of the service providers. Inclusion criteria were: consent, 40-74years, BMI ≥25kg/m2, ‘pre-diabetes’, and readiness to lose weight. Collaborative Care included both GP Mental Health Treatment Plan (GPMHTP) items (for depression, includes ≤10 individual psychological services/year) and Chronic Disease Management Plan (CDMP) items (for pre-diabetes, includes ≤5 individual allied health services/year) covered by Medicare for preparation of two separate but integrated, concurrent care plans.
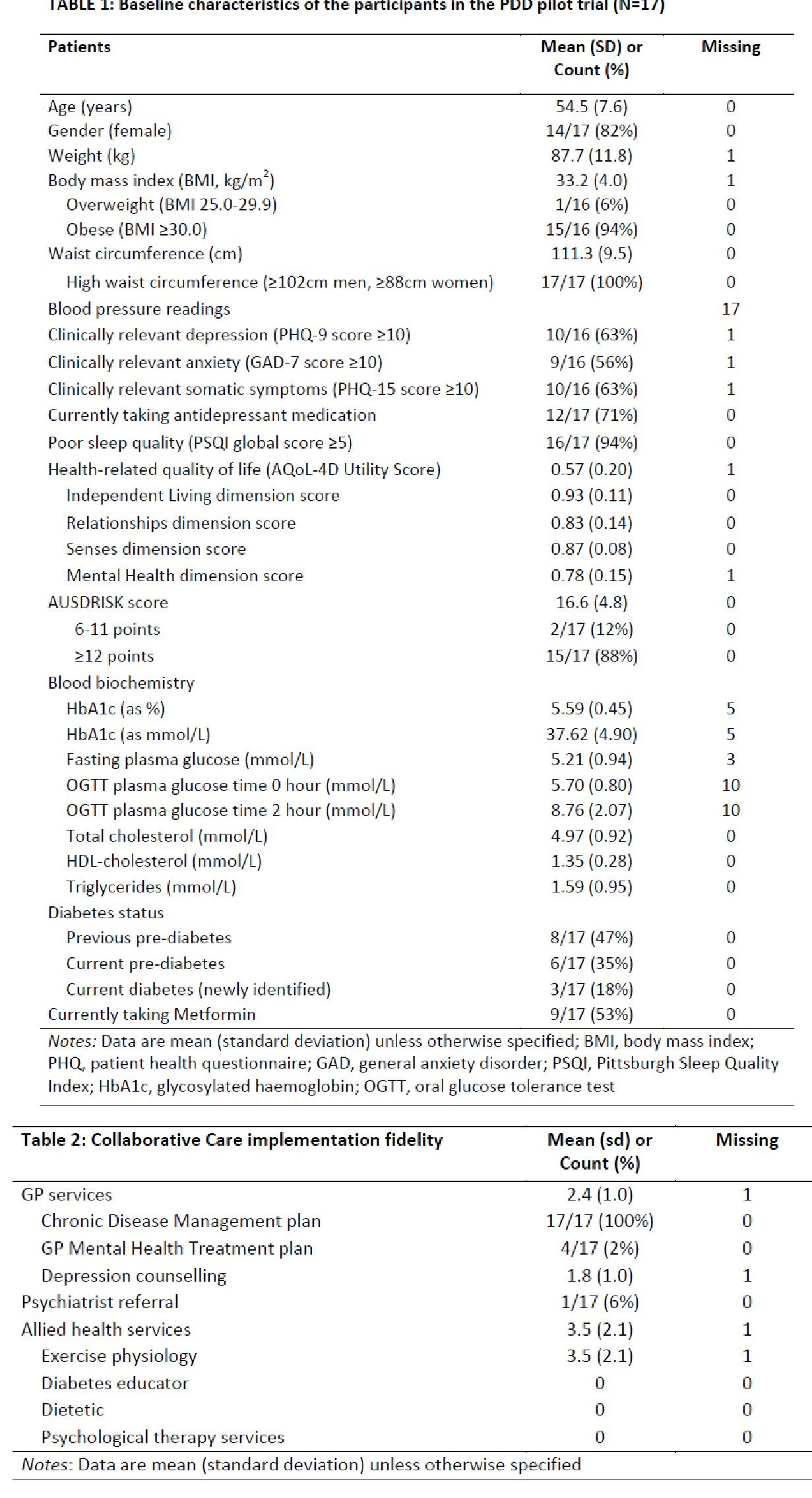
Results: 17 of 45 (38%) potentially eligible participants (meeting pre-screening age and pre-diabetes criteria) were recruited primarily during face-to-face routine consultations, of whom 16/17 (94%) participants attended the 12-week post-test clinic. Tables 1-2 show baseline characteristics and intervention fidelity data. GP reasons for not providing referrals for psychological services include lack of awareness of, and confidence in, their ability to effectively manage depression and modify unhealthy lifestyle behaviours; negative assumptions about the cost and time burden; and stigma of seeing a psychologist. The exercise physiologist observed “better” outcomes vs. usual care patients.
Conclusions: Our pilot data suggest future full-scale research on Collaborative Care for diabetes prevention in primary health care appears feasible in terms of recruitment and retention, although effective implementation requires strategies on facilitating: 1) assessment procedures; 2) integration of GPMHT and CDM plans; and 3) referrals to access allied health services, especially psychologists, for enhancing treatment fidelity.