Poster Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2016
Efficacy of an intensive and integrated team-based model of care for severely obese patients with type 2 diabetes in a public hospital setting (#267)
Background: We investigated the efficacy of an intensive team-based model of care for clinically meaningful weight loss and improvement in metabolic control in predominately severely obese patients with T2D over 12 months (m) of treatment.
Methods: We analysed retrospective data extracted from medical records for 53 obese patients with T2D patients who completed ≥12m of the Metabolic Rehabilitation Programme (MRP) during 2009-14. The MRP team included an endocrinologist, diabetes educator, dietitian, exercise physiologist (for supervised ≥moderate-intensity compulsory exercise), physiotherapist, podiatrist (2012-14), and psychologist (for barriers to healthy behaviour modification), co-located in the clinic and on the same day. Patients had initial consultations followed by regular clinics for review where necessary. The endocrinologist focused on weight loss rather than glucose lowering medications for achieving metabolic targets. The exercise physiologist was available daily (weekdays) for supervised individualised exercise programmes. Important clinical outcomes were changes in weight (kg), HbA1c (as %) and (SBP, mmHg) at 3, 6 and 12m.
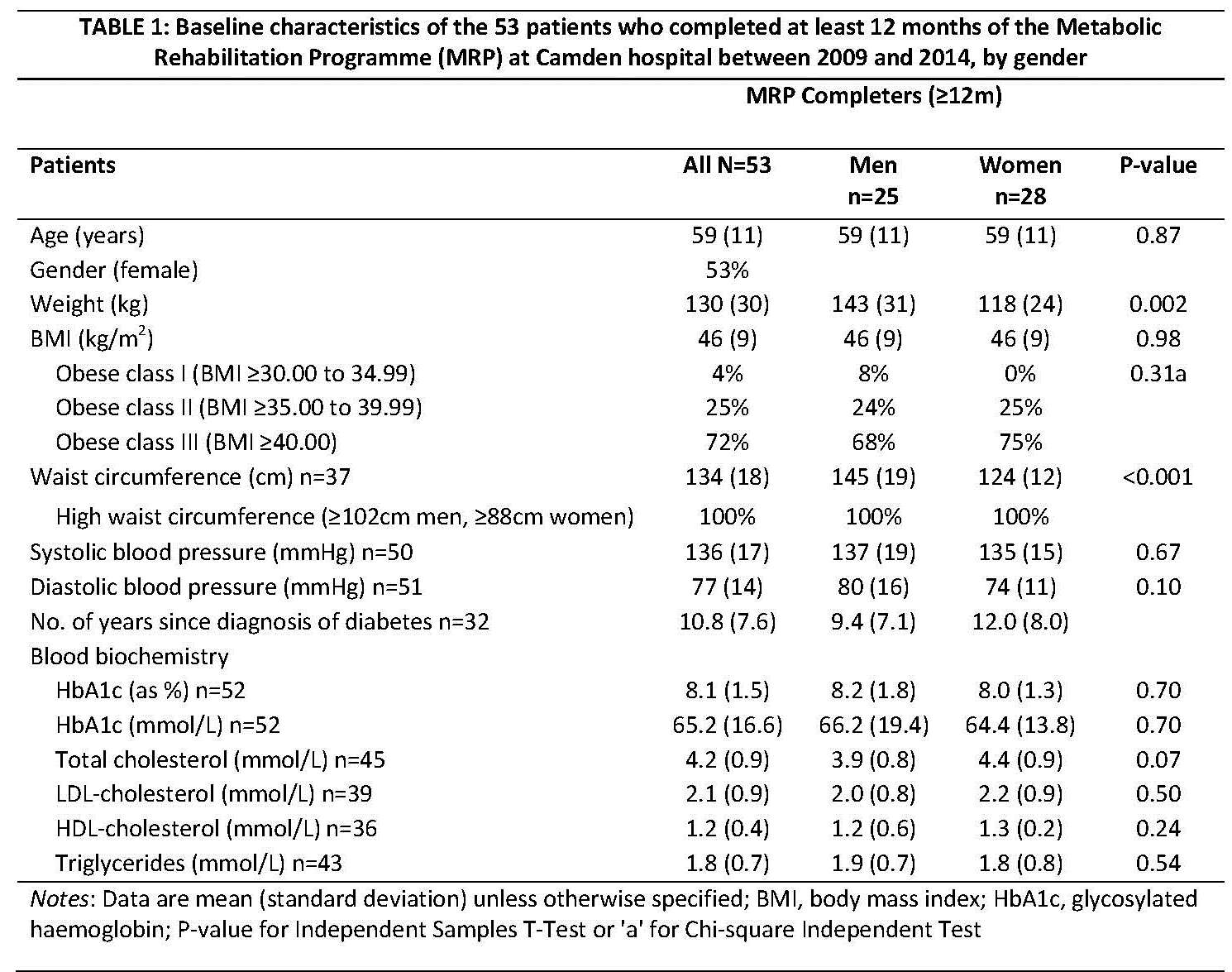
Results: Table 1 presents baseline characteristics. Within-group mean decrease (95% confidence intervals) in weight was 5.5kg (4.4,6.6), 8.6kg (7.1,10.1), and 11.6kg (9.6,13.5); in HbA1c was 0.8% (0.5,1.1), 0.9% (0.6,1.2), and 1.0% (0.7,1.4); and in SBP was 5.9mmHg (-0.1,11.8), 5.7mmHg (-1.0,12.3), and 10.0mmHg (6.0,13.9), at 3, 6, and 12m, respectively. Weight loss did not predict change in metabolic control. Higher baseline values predicted greater changes in outcomes: per 10kg predicted 12kg (6.6,17.8) weight loss; per 1% HbA1c predicted 0.5% (0.3,0.7) reduction; and per 10mmHg SBP predicted 5mmHg (2.8,7.7) reduction. There were no serious adverse events attributable to the MRP.
Conclusions: The MRP caused clinically meaningful and incremental weight loss and improvements in metabolic control at 3, 6, and 12m. Future research on the benefits and incremental costs of the MRP for management of complex T2D compared with standard Diabetes Clinic care is justified.